Case Study: Lab Incidents
 Ever since the SARS outbreak ended, there has been fear of new SARS cases triggering the same massive outbreak that killed
and infected so many people.
Ever since the SARS outbreak ended, there has been fear of new SARS cases triggering the same massive outbreak that killed
and infected so many people.
That fear resurfaced in September 2003 when a 27-year-old lab researcher in Singapore contracted SARS. Another near similar
case happened in December 2003 when a 44-year-old Taiwanese military scientist (referred to as Lt. Col. Chan), became
infected with SARS during a lab experiment. Fortunately, both were isolated cases of SARS.
In this case study, we will take a look at the two lab incidents involving SARS which happened in 2003. We will do compare
and contrast, and find out what steps can be taken to prevent such cases from happening again in the future.
Below all content of this page is listed by header title. Click on the link to go to a particular part within this page.
At anytime you can return to this list by clicking on 'Content Outline' at the end of each part.
Singapore case
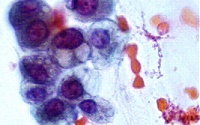
- The researcher worked in the Environmental Health Institute (Singapore) laboratory on 23 August 2003.
- The frozen West Nile virus sample he worked on was contaminated by the SARS virus.
- Virus sample taken from him closely matched the SARS virus strain in the lab.
- The man did not dress appropriately to work with high-risk samples.
- The man fell in on 26 August 2003.
- Over the following week, he saw a doctor, then went to Singapore General Hospital's (SGH) accident and emergency
department and saw a Chinese physician too.
- He was again admitted to SGH on 3 September as he had fever, muscle aches and joint pains.
- On 8 September 2003, SARS test results came back positive and he was moved to the new Communicable Disease Centre 2 at
Tan Tock Seng Hospital (Singapore).
Taiwan case
- The Taiwanese researcher probably caught the virus when he handled a torn trash bag that leaked contaminated liquid on
5 December 2003.
- The scientist then traveled to Singapore to attend a conference from December 7 to December 10.
- He returned to Taiwan at about noon on December 10. He began to feel sick that day and immediately knew to place himself
at home in quarantine.
- On December 16, he phoned for an ambulance and was admitted to a local hospital with a fever.
On 9th September 2003, Singapore shares plunged to a one-month low with the benchmark Straits Times Index falling 42.14
points, or 2.6 per cent, to 1,580.14.
Singapore case
- The related labs were closed.
- Four experts from the World Health Organization and the Centers for Disease Control and Prevention in America flew to
Singapore to make checks on the laboratories where the researcher who caught Sars had worked.
- WHO officials helped the Health Ministry to investigate the practices, facilities and equipment at the Environmental
Health Institute laboratory at Science Park II and the microbiology laboratory at the National University of Singapore
(NUS).
- Tightened screening at airports in Hong Kong and Taiwan.
Taiwan case
- In Singapore, 70 people were ordered into quarantined.
- In Taiwan, control level for SARS precaution was raised from level zero to the more stringent level B by the special
SARS committee. The control level will return to level zero if no new cases are detected in the following 21 days.
- Taiwan CDC initiated fever monitoring in government institutions and schools.
- Travelers with fever will be restricted from leaving Taiwan and will be required to obtain a health certificate from
a hospital.
- All laboratories, in Taiwan, which work on the SARS-CoV culture were ordered to undergo stringent disinfection
procedures and all research on viral cultures were suspended until biosafety has been guaranteed and approved by the
government.
- There is no doubt that both isolated cases of SARS arising from lab incidents could have been prevented if safety had
been the number one issue.
- Many laboratories around the world have stored hundreds of SARS specimens in freezers, ready to be thawed as needed. The
WHO has cautioned countries that accidents may occur in laboratories where there is little experience with dangerous
infectious agents.
- In today's medical world, some workers do not practice biosafety measure. As some experts put it, "doing the research is
more important than doing the research safely".
This is not the first time in medical history that failures in biosafety standards have resulted in lab incidents.
For example, a notorious accident occurred in 1979 when the smallpox virus escaped from a laboratory at the University of
Birmingham in England. It infected two people, one fatally, months after epidemiologists had rid the world of smallpox.
Although no additional spread occurred, the scientist in charge of the laboratory committed suicide.
- Salma Khalik. It's SARS, but 'an isolated case' - SEPT 10, 2003. The Straits Times Interactive. (10 September
2003). [Online]. Available:
http://straitstimes.asia1.com.sg/sars/story/0,4395,209090,00.html?
[25 January 2004]
- Ben Nadarajan . 'I'm Sars positive' - SEPT 10, 2003. The Straits Times Interactive. (10 September 2003).
[Online]. Available:
http://straitstimes.asia1.com.sg/sars/story/0,4395,209088,00.html?
[25 January 2004]
- WHO and US experts to fly in to help check labs - SEPT 12, 2003. The Straits Times Interactive. (12 September
2003). [Online]. Available:
http://straitstimes.asia1.com.sg/sars/story/0,4395,209413,00.html?
[25 January 2004]
- Latest SARS case tracked to lab accident - SEPT 24, 2003. The Straits Times Interactive. (24 September 2003).
[Online]. Available:
http://straitstimes.asia1.com.sg/sars/story/0,4395,211277,00.html?
[25 January 2004]
- Infected man in Taiwan has not spread SARS virus. People's Daily Online. (19 September 2003). [Online].
Available:
http://english.peopledaily.com.cn/200312/19/eng20031219_130737.shtml
[25 January 2004]
- Officials Concerned About SARS Infections by Lab Contamination. [Online]. Available:
http://www-tech.mit.edu/V123/N44/sars_long5_44.44w.html
[25 January 2004]
- Taiwan Lab Worker Recovering from SARS. The HealthScout Network. (19 December 2003). [Online]. Available:
http://www.healthscout.com/news/68/1503296/main.html
[25 January 2004]
- Confirmed SARS case in research laboratory in Taiwan - December 17 2003. Department of Health, Taiwan, R.O.C.,
SARS Online Information Center. [Online]. Available:
http://sars.doh.gov.tw/news/2003121701.html [6 February 2004]
|

|